Maintenance therapy with Lenalidomide or proteasome inhibitors after autologous stem cell transplantation (ASCT) in multiple myeloma (MM) is an important component of first line treatment, resulting in deepening response (DR), converting PR to VGPR/CR or VGPR to CR in most patients and, in significantly longer PFS and OS. Of note, randomised clinical trials and real-world data confirm that DR also occurs in about 30% of patients receiving placebo or no maintenance at all.
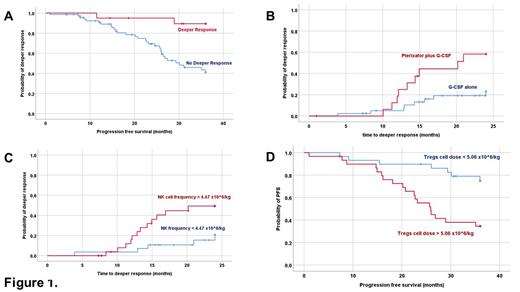
We analysed 90 patients with MM treated with first line ASCT in Hammersmith Hospital between 2017 - 2020, who did not receive maintenance therapy. We observed DR in 20 patients (22%) in the first two years. Patients achieving a DR had significantly higher PFS at 36 months post ASCT (89.4% v 41.1%, p=0.001 - Figure 1A). Baseline and ASCT characteristics, including high-risk cytogenetics, ISS, induction therapy and conditioning were comparable in DR and non-DR patients, however the use of the CXCR4 antagonist Plerixafor plus G-CSF vs G-CSF alone in the mobilisation regimen was associated with a higher probability for DR in the first 24 months post ASCT (58.3% v 23.2%, p=0.011 - Figure 1B).
We suggest that improvement in depth of response after ASCT without pharmacological intervention indicates an immune anti-MM effect, underpinned by the immune composition of autologous grafts.
We used 14-colour flow cytometry to analyse the immune cell frequencies in graft in 59 of the above patients, including 17 patients mobilised with Plerixafor plus G-CSF and 42 with G-CSF alone. The cell dose of each cell population was calculated from the relative frequency of CD34 cells in the graft and the CD34 cell dose infused in ASCT. In line with previous reports, the use of Plerixafor results in higher frequency and cell dose (in x10^6 cells/kg) of T cells in the graft (70.6% v 61.3%, p=0.015 and 306.2 v 161.4, p=0.007), driven mostly by a higher frequency (67.8% v 48.7%, p= 0.001) and dose (224 v 78.2, p=0.001) of central memory (CM) CD4 T cells. On the contrary, frequency and cell dose of effector memory (EM) CD4 T cells in Plerixafor plus G-CSF mobilised grafts were lower (6.7% v 21.5%, p=0.006 and 15.5 v 34.7, p=0.063). Apart from mobilisation regimen, univariate analysis showed a higher probability of achieving DR in grafts with high frequency of CD4 CM T cells (p= 0.012), NK cells (p=0.018 , Figure 1C), CD8 CM cells (p=0.06), higher dose of CD8 memory stem cells (p=0.033), lower frequency and dose of CD4 EM (p= 0.017 and p=0.007) and a lower dose of CD4 terminal effectors (TE) (p=0.039). In multivariate analysis, only a high NK cell frequency (p=0.011) and low CD4 TE cell dose (p=0.01), driven by their PD1 expression, predicted a higher probability for DR.
Tregs frequency and cell dose were not affected from mobilisation regimen. However, Tregs dose was the stronger predictor of PFS at 36 months (75% with dose <5.06 x10^6/kg v 34.5% with dose >5.06 x10^6/kg, p= 0.001). Similarly, lower cell doses of CD4 EM (p=0.012) and frequency of CD4 TE (p=0.034) predicted a higher probability of PFS, but only Tregs cell dose retained significance in multivariate analysis (Figure 1D, p=0.001).
In conclusion, spontaneous DR occurs in the first 2 years post ASCT in the absence of maintenance therapy and is associated with better PFS. CD4 memory subsets and NK cell graft composition appears significant for a potential immunological effect in DR. Additionally, a lower cell dose of immunosuppressive Tregs appears more important for sustaining long-term remission post ASCT.
Disclosures
Bazeos:Roche Products: Current Employment.